Alternative healing methods put to the test: What do science and patients say?
Explore the effectiveness of alternative healing methods such as homeopathy, acupuncture and herbal medicine based on scientific evidence and patient experiences.

Alternative healing methods put to the test: What do science and patients say?
In a world where modern medicine often takes center stage, many people are looking for alternative ways to promote their health and relieve discomfort. Methods such as homeopathy, acupuncture and herbal medicine have found followers over centuries and are deeply rooted in various cultures. But while the popularity of these approaches appears to be unbroken, questions remain about their actual effectiveness and scientific basis. Can these traditional practices keep up with the rigorous standards of evidence-based medicine, or are their effects based primarily on faith and placebo? This article takes a critical look at the healing methods mentioned, highlights current research results and attempts to draw the boundaries between traditional knowledge and demonstrable effects. Immerse yourself in a differentiated view that takes both historical roots and modern analyzes into account.
Introduction to alternative healing methods

Imagine entering a pharmacy or health food store and being greeted by a colorful assortment of herbal teas, essential oils and homeopathic globules. This diversity reflects how deeply anchored alternative healing methods are in our society today. From Traditional Chinese Medicine (TCM) to Indian Ayurvedic healing – the range of approaches that are used as a supplement or alternative to conventional medicine is impressive. Many people resort to these methods, be it out of curiosity, cultural connection or the hope of gentler treatment options. According to an overview Wikipedia Demand has increased significantly in recent decades, especially in western countries, where around 1.7 billion euros were spent on special therapeutic drugs in Germany alone in 2018.
A look at the diversity shows how different the approaches are. Phytotherapy, i.e. the use of medicinal plants, ranges from teas and ointments to inhalations and baths to relieve symptoms such as colds or skin problems. Equally popular is acupuncture, a central component of TCM, which aims to harmonize life energy - the so-called Qi - by placing needles at specific points. Studies like them on Envivas mentioned indicate that acupuncture can have positive effects on complaints such as back pain or allergies. TCM herbal therapy is also very popular, often in combination with other methods such as cupping.
Ayurvedic medicine, which comes from India, takes a holistic approach and aims to bring body, mind and lifestyle into harmony. The aim is to achieve inner balance through diet, exercise and special treatments - a concept that fascinates many followers in Western countries. Research results suggest that Ayurveda can have a supportive effect on diseases such as high blood pressure or joint problems. Less tangible, but still widespread, is homeopathy, which is based on the principle of “healing like with like”. Highly diluted substances are supposed to stimulate the body to heal itself, but there is no scientific recognition - a point that repeatedly causes debate in society.
In addition to these well-known methods, there are also less common but still appreciated methods. Kneipp therapy, for example, uses water treatments, exercise and medicinal plants to strengthen the immune system, while aromatherapy with essential oils promotes well-being, often as an accompaniment to other approaches. Osteopathy, a manual therapy to support self-healing powers, is also particularly popular with children and adults with muscular problems. Less commonplace, but deeply rooted in history, are practices such as bloodletting or leech therapy, which are used to “clean” the blood in cases of high blood pressure or venous diseases.
Anthroposophical medicine follows a spiritual approach, which is based on Rudolf Steiner's philosophy and looks at people in their entirety. Mistletoe therapy is particularly well-known and is often used as an adjunct to cancer. Bach flower therapy also focuses on mental balance and is intended to harmonize emotional states with 38 different flower essences - even if scientific evidence is lacking. Methods such as Schüssler salts, which are based on a supposed mineral deficiency, or colon hydrotherapy for intestinal cleansing are also attracting interest, although their effect is not without controversy.
The popularity of all of these approaches shows how great the need is for alternative or complementary ways to promote health. Whether it is the gentle effects of medicinal plants, the holistic view of Ayurveda or the traditional acupuncture - many people value the opportunity to actively participate in their recovery. But behind the fascination with these methods lurks the question of how much of it is based on actual effects and how much is based on expectations.
Homeopathy in focus

Have you ever wondered how a tiny ball of sugar, barely larger than the head of a pin, can promise healing? This is exactly where homeopathy comes in, an approach that has caused both fascination and skepticism for over two centuries. Developed at the end of the 18th century by the German doctor Samuel Hahnemann, this system is based on a basic idea that initially seems paradoxical: a substance that triggers certain symptoms in healthy people should, in a highly diluted form, alleviate those same symptoms in sick people. This principle, known as “similia similibus curentur” – like is cured by like – is at the heart of this alternative healing method.
The production of homeopathic remedies follows a very specific ritual. Raw materials, which come from plants, animals or minerals, are repeatedly diluted and shaken in a process called potentization. Often the dilutions are so extreme that at the end there are no detectable molecules of the original substance left - a point that is often criticized in the scientific community. Nevertheless, adherents believe that this process transmits a type of “energetic information” that stimulates the body to heal itself. Such preparations, often in the form of globules or drops, are then taken orally to treat a variety of ailments, from colds to chronic illnesses.
In practical use, homeopathy places great emphasis on an individual approach. A visit to a homeopathic practitioner usually begins with a detailed anamnesis that goes far beyond the pure physical symptoms. The patient's emotional states, living conditions and personal characteristics play a central role, as the treatment is aimed not only at the disease but at the whole person. These conversations can last anywhere from ten minutes to over an hour, as shown in an overview Wikipedia is described. The aim is to find a remedy that exactly matches the individual symptoms and personality of the person affected - a process that for many patients represents a welcome change from conventional medicine, which is often perceived as impersonal.
The application of this method extends to a wide range of conditions. People often turn to homeopathic remedies for everyday problems such as colds, allergies or sleep disorders. Its use is particularly popular with children, for example to relieve teething pain or minor infections, as the preparations are considered gentle and have no side effects. They are also widespread in self-medication - an analysis from the USA shows that many adults use homeopathic products without consulting a practitioner, especially for colds or musculoskeletal pain, as shown on the website NCCIH mentioned. But there are also cases in which homeopathy is used for more serious illnesses as a supplement or even alternative to conventional therapies, which is not without risks.
Hahnemann himself introduced the concept of “miasms,” a type of underlying cause of chronic disease that should be treated by homeopathic remedies. This idea, which is based on a non-scientifically based idea of the causes of disease, shows how homeopathy is strongly influenced by a philosophical rather than an empirical basis. Nevertheless, it has found supporters worldwide, from Europe to North America to India, where it is even integrated into the national health system. Its popularity peaked in the 19th century, followed by a decline, before experiencing a renaissance in the wake of the New Age movement of the 1970s.
However, the practical application raises questions that go beyond the mere production and consumption of the funds. How can a preparation that, chemically speaking, often only contains sugar or water, have an effect? And why do so many users report positive experiences even though the scientific evidence speaks against it? This discrepancy between personal perception and objective research forms a central conflict that accompanies homeopathy to this day.
Scientific evidence on homeopathy

Questioning the effectiveness of a healing method based on principles as unusual as extreme dilutions opens up a wide field of debate and data. Homeopathy has been under the microscope of science since its inception, and numerous studies and comprehensive meta-analyses have attempted to evaluate its actual effects. What emerges is a picture that may be disappointing for many supporters, while for critics it provides long-awaited confirmation. The question of whether homeopathic remedies produce more than just a placebo effect remains a central point of contention in medical research.
A closer look at the scientific study of this method reveals a clear trend. Extensive clinical studies that have been carried out over decades have predominantly come to the conclusion that homeopathic preparations have no specific effect beyond the placebo effect. One of the most comprehensive reviews comes from Australia, where the government concluded in 2015 that there was no reliable evidence of the effectiveness of homeopathy for any health condition after an analysis of 57 systematic reviews and 176 individual studies. These results, as they appear on the website of NCCIH summarized, underline the difficulty of demonstrating a therapeutic effect that goes beyond patients' expectations.
Meta-analyses, which combine a variety of studies to draw more reliable conclusions, paint a similar picture. In the 21st century, such summaries have repeatedly shown that the basic principles of homeopathy - particularly the idea that highly diluted substances have a healing effect - are incompatible with the fundamental laws of chemistry and physics. Many of these analyses, such as in an overview Wikipedia presented, come to the conclusion that positive results in individual studies are often due to methodological weaknesses, small samples or biases. As soon as stricter scientific criteria are applied, evidence of a specific effect disappears.
Another aspect that is repeatedly highlighted in research concerns the biochemical composition of the preparations. Since many homeopathic remedies are so diluted that molecules of the original substance can no longer be detected, there is no plausible explanation as to how they could have a pharmacological effect. Scientists argue that the reported improvements in patients are more likely due to psychological factors such as the placebo effect, natural recovery or concomitant treatments. This view is shared by major health organizations, who emphasize that there is no reliable evidence of the effectiveness of homeopathic remedies.
Nevertheless, there are also isolated studies in research that suggest positive effects, especially for subjective complaints such as pain or sleep disorders. However, critics point out that such results are often not reproducible and are not confirmed in larger, more controlled studies. The discussion is further complicated by the fact that many users use homeopathic remedies in combination with other therapies, which makes it difficult to assign effects. In addition, intensive care from practitioners, who often spend a lot of time taking anamnesis, plays a role in the perception of improvement - a factor that can be independent of the effect of the medication itself.
The scientific debate has also had political and regulatory consequences. In countries such as Australia, Great Britain and France, government funding for homeopathic treatments was stopped because the evidence for their effectiveness was deemed insufficient. Such decisions reflect the broad consensus in research that resources would be better invested in proven effective therapies. But despite these developments, homeopathy remains present in the public, supported by personal reports and a deep-rooted skepticism towards conventional medicine among some people.
The discrepancy between individual perception and scientific evaluation leads to ongoing tension. As studies and analyzes continue to question the fundamentals of homeopathy, many users are looking for explanations for their own positive experiences. This gap between subjective experience and objective data opens up space for further questions that concern other alternative approaches beyond homeopathy.
acupuncture

Let's travel back in time, thousands of years ago, to a world where the art of healing was closely linked to the philosophy of life. In this context, a method emerged in China that is still practiced worldwide today: acupuncture. Its roots go back to around 100 BC. BC, when it was developed as part of Traditional Chinese Medicine (TCM). This practice is based on the idea that an invisible life energy, called Qi, flows through special pathways in the body called meridians. When this energy flow is disrupted, illness can arise, and this is exactly where acupuncture comes in to restore balance.
The basic idea behind this technique is to harmonize the flow of Qi by specifically placing thin needles at specific points along the meridians. These points, of which there are hundreds on the body, are said to be related to different organs, emotions, or physical functions. From the perspective of TCM, stimulating these areas not only regulates the flow of energy, but also activates the body's self-healing powers. In Western understanding, however, it is often assumed that the needles stimulate nerves, muscles and connective tissue, which could promote the release of natural painkillers such as endorphins, as is the case on the side of the Mayo Clinic is explained.
The practical implementation of an acupuncture treatment follows a clear process, although this can vary depending on the practitioner and cultural background. First, a detailed medical history is taken, during which the patient's symptoms, lifestyle and general health are discussed. The patient then lies on a padded bed while the practitioner inserts thin, sterile stainless steel needles into the selected points. These needles, typically used between 5 and 20 per session, are inserted at different depths depending on the intended effect. Often, needle placement is virtually painless, with some patients experiencing a slight tingling or dull sensation - known as "de-qi" - which is considered a sign of correct placement.
In addition to the classic needle technique, there are also variations that are intended to enhance the effect. Some practitioners apply heat by heating the needles or using a technique called moxibustion, in which dried mugwort is burned near the skin. Others combine the treatment with electrical pulses, known as electroacupuncture, to intensify the stimulation. Methods such as acupressure, which uses pressure instead of needles, or auriculotherapy, which focuses on points on the ear, are also part of the expanded repertoire. This diversity shows how adaptable the practice has become over the centuries.
Historically, this healing art spread from China to Korea in the 6th century, later to Japan and finally to Europe, where it first became known through medical missionaries. Today it is used in many countries, including the United States, Australia and numerous European nations, often in combination with other therapies. Treatment duration varies, with one session lasting up to 60 minutes, and 6 to 8 sessions are often recommended to achieve noticeable results. The areas of application are wide-ranging - from relieving chronic pain such as back pain or migraines to supporting nausea, for example after chemotherapy, or respiratory diseases such as allergic rhinitis.
The safety of the method depends heavily on the qualifications of the practitioner. If done correctly and using sterile disposable needles, the risks are low, although mild side effects such as pain, minor bleeding or bruising may occur. Particular caution is required in certain groups of people, such as pregnant women, as some points could trigger contractions, or in people with pacemakers when electrical stimulation is used. Nevertheless, acupuncture remains an attractive option for many, not least because of its minimally invasive nature and the individual care that is often perceived as beneficial.
The long history and worldwide spread of this technology raise questions that go beyond mere application. How can we explain the success that many patients report and to what extent do cultural beliefs play a role in the perception of the effect? These considerations inevitably lead to a deeper examination of the evidence behind acupuncture.
Evidence on acupuncture

A small prick that is supposed to bring great relief - this idea drives many people to try acupuncture as a remedy for pain or other complaints. But what does science say about the actual effects of this millennia-old practice? Over the past few decades, research on this topic has increased significantly, with thousands of studies attempting to evaluate effectiveness in a variety of conditions. The results are as diverse as the areas of application themselves, which further fuels the discussion about the true benefits of this method.
Over 10,000 randomized controlled trials of acupuncture have been published since 1975, and more than 2,400 systematic reviews have appeared between 2000 and 2020, according to a comprehensive analysis PMC shows. The focus of these studies is often on musculoskeletal problems, which account for approximately 35% of studies, followed by neurological diseases, cancer and cardiovascular problems. The effect on chronic pain is particularly frequently examined, with some reviews finding moderate to strong effects on non-specific back pain, neck and shoulder pain and fibromyalgia. These results suggest that needle stimulation may provide noticeable relief in certain cases.
A recent overview, published as an open access article and funded by SMS, also highlights positive developments, such as TCM.edu reported. This analysis of meta-analyses and systematic reviews from 2017 to 2022 shows evidence-based effectiveness for ten medical indications. These include chronic pain, back pain, knee osteoarthritis, migraines, tension headaches, postoperative nausea and vomiting, cancer-related fatigue, menopausal symptoms, female infertility (in combination with reproductive therapies), and chronic prostatitis or pelvic pain syndrome. In addition, there is evidence of potential benefit in 82 other indications, while no or insufficient effect has been demonstrated in only six.
Despite these encouraging data, the research is not without challenges. A frequently cited problem is the quality of many studies, particularly with regard to methodological weaknesses such as missing exclusion criteria or insufficient consideration of publication bias. In addition, the design of placebo-controlled studies makes it difficult to clearly assign effects, as so-called sham acupuncture - in which needles are placed in non-specific points - often shows similar results to the real treatment. This raises the question of whether the effect is based on the patient's expectations or on unspecific stimulation.
Another aspect that receives attention in research is the geographical origin of the studies. Over 40% of systematic reviews come from China, raising concerns about possible bias or cultural influences on the results. Nevertheless, western studies, for example from the USA or Great Britain, have also documented positive effects on certain complaints such as migraines or postoperative nausea. This discrepancy between study quality and origin shows how important international collaboration and standardized methods are for future research.
What is also interesting is that despite the growing evidence, the integration of acupuncture into healthcare systems often lags behind. In many countries, insurance only covers treatment to a limited extent, usually only for painful illnesses. Underfunded research areas such as use in depression, migraine or opioid addiction also offer potential for further insights, particularly given the high burden of disease in these areas. Suggestions for improvement include digitization of evidence, exchange between clinicians and decision-makers, and joint research efforts to make better use of existing data.
The studies' mixed results reflect the complexity of evaluating a method based on both historical beliefs and modern scientific standards. While some patients report noticeable improvement, the question remains as to how much of this is due to specific mechanisms and how much to other factors. This uncertainty leads directly to further consideration of alternative approaches that also balance tradition and evidence.
Herbal medicine

Even before written records existed, people turned to nature for healing - evidence of the deep connection between humans and plants that continues to the present day. Archaeological evidence suggests that even Neanderthals used medicinal herbs around 60,000 years ago, and since then herbal medicine, also known as phytotherapy, has developed across cultures and continents. From the ancient civilizations of Egypt, China and Greece to the medieval herb gardens of Europe, the use of medicinal plants to relieve ailments and prevent disease is a universal heritage that is now experiencing a renaissance.
In many societies, the use of herbal remedies was and is deeply rooted in tradition. According to the World Health Organization (WHO), 70 to 95% of the world's population is treated by traditional medicine, as stated on the site of Susan Kaiser is highlighted. In China, for example, herbs are a central component of Traditional Chinese Medicine (TCM), where they are often used in complex mixtures to harmonize the body. In India, herbal medicine plays a key role in Ayurveda, where plants such as turmeric or ashwagandha are not only considered medicinal, but also as a means of strengthening the entire organism. In the Western context, especially in Europe, herbs were cultivated in monastery gardens in the Middle Ages in order to preserve and pass on knowledge about their effects.
The uses of medicinal herbs are as diverse as the cultures from which they come. They are often taken internally as teas, tinctures, decoctions, capsules or tablets to treat ailments such as digestive problems or sleep disorders. They are used externally in the form of baths, inhalations, compresses or oil mixtures, for example to relieve skin irritation or muscle tension. While Ayurvedic practices often rely on complex oil extracts, Western herbal medicine often prefers aqueous extracts or baths. These differences reflect not only regional preferences, but also individual perceptions of health and healing.
A notable aspect is customization, which plays a role in many traditions. In modern herbalism, a detailed medical history is often performed to identify weaknesses in the immune system or specific ailments before tailor-made blends are created. This approach can also be found in shamanistic practices, where plants are said to have not only a physical but also a spiritual effect. Dosage varies greatly - while some cultures rely on gentle, long-term applications, others prefer concentrated preparations for quick effects, highlighting the need for expertise and caution.
Herbal medicine has been scientifically classified since the 19th century, when active ingredients such as morphine were isolated from the opium poppy or salicin from willow bark, leading to the development of modern medicines. Nevertheless, the traditional application remains alive, often in combination with new findings. In Germany, for example, phytotherapy is officially integrated into the healthcare system and is subject to strict regulations to ensure quality and safety. In other regions, however, such mechanisms are missing, which sometimes makes their use risky as quality standards and dosage recommendations are not always adhered to.
The cultural significance of medicinal herbs goes far beyond their medicinal effects. In many communities they are part of rituals and traditions that pass knowledge from generation to generation. Whether it's chamomile, used for centuries in Europe to combat anxiety and inflammation, or ginseng in Asia, considered a tonic, plants are often more than just remedies; they embody a connection to nature and history. This emotional and spiritual dimension makes its use particularly valuable for many people.
However, its widespread use also raises questions, particularly regarding safety and interactions with conventional medications. How can ancient knowledge be reconciled with the requirements of modern medicine, and which plants stand up to scientific scrutiny? These considerations lead us to look at the evidence and the actual effectiveness of medicinal herbs.
Scientific studies on herbal medicine

Viewing nature as a pharmacy may sound romantic, but how much truth is there in the healing promises of herbs that have been valued for centuries? Modern research has begun to scrutinize the traditional knowledge of herbal medicinal herbs to evaluate their therapeutic effects with scientific precision. From double-blind studies to laboratory tests, the results are as diverse as the plants themselves, offering both confirmation and challenges for application in today's medicine. This look at the evidence shows that not every herb delivers what it promises, but some have surprising potential.
One of the most frequently studied plants is St. John's wort, known for its mood-enhancing effects. Studies like them on Planted mentioned suggest that it may help mild to moderate depression by affecting serotonin levels in the brain. Clinical studies show that standardized extracts in some cases achieve results comparable to synthetic antidepressants, but with fewer side effects such as fatigue. However, researchers warn against interactions because St. John's wort can reduce the effectiveness of other medications, such as birth control pills, underscoring the need for professional advice.
The effects of chamomile, which has long been valued for its calming properties, are also well documented. Research suggests that it can help with sleep disorders and mild anxiety, thanks to its anti-inflammatory and antispasmodic properties. The situation is similar with peppermint, whose essential oils have been shown in studies to provide relief from digestive problems such as irritable bowel syndrome. These effects are attributed to the spasmolytic action that reduces muscle spasms in the gastrointestinal tract, making it a popular choice for everyday ailments.
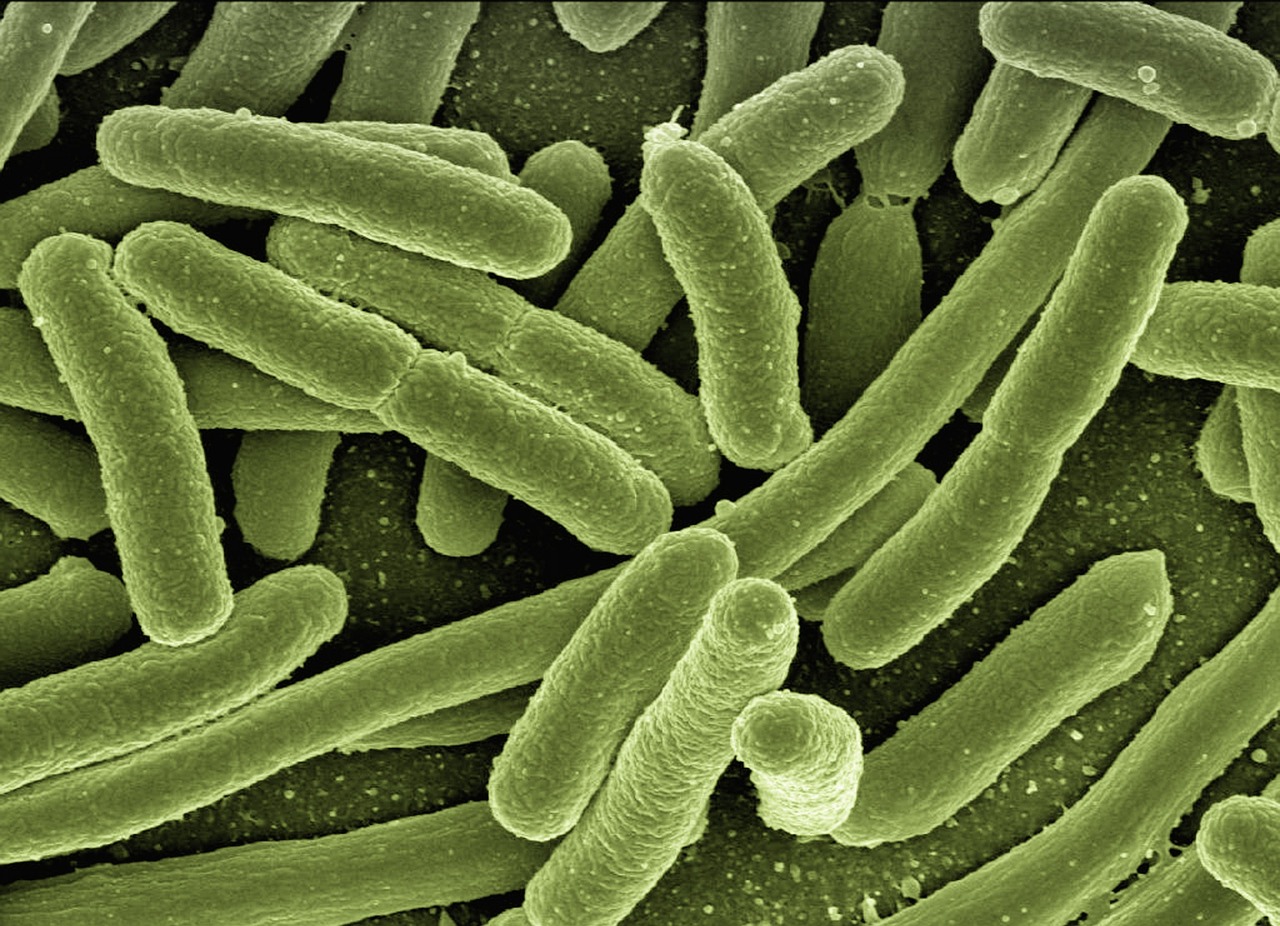
Another herb that has recently gained attention is turmeric, whose active ingredient curcumin shows promising antibacterial properties. Laboratory tests, such as those on SciSimple show that curcumin can inhibit the growth of bacteria such as Staphylococcus aureus and Escherichia coli by disrupting their protein production. In some experiments it achieved comparable results to common antibiotics, although the effectiveness depends heavily on the extraction method. These results suggest potential, particularly in combination with conventional antibiotics, to combat resistance, although clinical trials in humans are still pending.
The study of cactus extracts, especially Opuntia ficus-indica, which could be effective against resistant bacteria such as Pseudomonas aeruginosa, a common problem in hospitals, also provides interesting findings. Research shows that antibacterial activity increases when extracts are heated and positive effects can be achieved even in low concentrations. In contrast, the results for flaxseed were less convincing - although rich in healthy fats and nutrients, it actually promoted bacterial growth in some tests, limiting its role to a supportive rather than primary effect.
In addition to these promising examples, there are also herbs for which the evidence is mixed or contradictory. Ginkgo biloba, often promoted for improving cognitive function, has shown slight benefits for memory problems in some studies, while others have found no significant effects. It also increases the risk of bleeding when taking blood thinners at the same time, which complicates their use. Similar caution should be exercised with ginger, which, although it relieves nausea and has an anti-inflammatory effect, can cause stomach irritation in high doses.
Research faces several challenges, including variability in the quality of extracts and the need to determine optimal dosages. Many studies have so far been limited to laboratory experiments, and the transfer to the human organism requires further clinical investigations. Nevertheless, the growing number of studies shows that medicinal herbs could make a valuable contribution in certain areas, especially when synergies with conventional therapies are used. What role these herbal remedies ultimately play in modern medicine depends on further standardization and education.
Comparison of alternative healing methods

Three paths to healing, but each takes a different direction - homeopathy, acupuncture and herbal medicine offer different paths to promote well-being, yet face the same challenge: proving their effectiveness in a world driven by scientific evidence. These alternative approaches, deeply rooted in historical traditions, differ fundamentally in their philosophy, methodology and the way they address the human body and mind. A comparison of their concepts and supporting research reveals both similarities and striking differences that illuminate their respective roles in the modern healthcare landscape.
Let's start with homeopathy, whose core idea rests on a principle of similarity. Developed in the late 18th century, it assumes that a substance that causes symptoms in healthy people can, in highly diluted form, bring relief to sick people with similar symptoms. The production of these agents by repeated dilution and shaking often results in no detectable molecules of the starting substance remaining - a point that has attracted much criticism in science. Applications range from treating allergies to skin problems to psychological conditions such as anxiety. However, despite its popularity and the personalized care that many patients value, evidence remains sparse. Extensive meta-analyses, as documented on various platforms, usually show no effect beyond the placebo effect, which often classifies homeopathy as pseudoscience in the scientific community.
Acupuncture approaches the goal of healing in a completely different way. With roots in Traditional Chinese Medicine (TCM) dating back over 2,000 years, it is based on the idea of a flow of energy, called Qi, that circulates through meridians in the body. Disturbances in this flow are said to cause disease, and by placing thin needles at specific points the balance is restored. This method is often used to relieve pain such as back pain or migraines, but also for psychological complaints such as depression or insomnia Difference.de described. In contrast to homeopathy, there are a growing number of studies that demonstrate moderate to strong effects in certain indications, such as chronic pain or postoperative nausea. However, research remains challenged by methodological difficulties and cultural differences in study quality, making the evidence not always clear.
A third approach is taken by herbal medicine, also known as phytotherapy, which is based on the use of medicinal plants or their components to treat complaints. This practice, one of the oldest medical therapies in the world, can be found in cultures ranging from TCM to Indian Ayurveda to European tradition. Preparations such as teas, tinctures or extracts aim to relieve physical and sometimes psychological suffering - from digestive problems with peppermint to sleep disorders with valerian. The scientific support varies greatly depending on the plant, as shown on Wikipedia shown. While some herbs, such as St. John's Wort for depression or turmeric for inflammation, show promising results, others are less well researched or have conflicting data. In addition, the standardization of ingredients, which depend on climate and harvest time, requires strict controls to ensure effectiveness and safety.
A direct comparison of the approaches reveals fundamental differences in their approach. Homeopathy relies on a philosophical foundation that often defies scientific explanation and focuses on highly individualized treatments without physical intervention. Acupuncture, on the other hand, uses a physical method – the placement of needles – and combines an energetic theory with measurable physiological effects such as nerve stimulation. Herbal medicine, on the other hand, relies on tangible, biochemically active substances whose effects are often closer to conventional medicines, but which can vary in quality due to natural fluctuations. These conceptual contrasts are also reflected in acceptance: While acupuncture and herbal medicine are at least partially integrated in many health systems, homeopathy often remains controversial and is no longer supported by the state in some countries.
The evidence further reinforces these differences. Acupuncture has a growing number of studies demonstrating specific benefits for pain and other conditions, although the mechanisms are not fully understood. Herbal medicine shows clear pharmacological effects with certain plants, but faces the challenge of standardization and the need for further clinical studies. Homeopathy, on the other hand, struggles with a lack of convincing evidence, with most analyzes finding no specific effect beyond placebo. This discrepancy raises the question of how much weight personal experiences should have compared to objective data.
The comparison of these methods shows that alternative healing approaches cannot be viewed as a monolithic block. Each brings its own history, philosophy, and evidence base that defines both its strengths and limitations. How these differences influence perception and application in practice leads to a broader discussion about the role of tradition and science in modern health care.
Patient experiences and reports
Behind every medical decision there is a personal story, an individual struggle or a spark of hope that often outweighs any study. When it comes to alternative healing methods, it is the experiences and opinions of patients that offer a vivid contrast to scientific analyses. From the search for relief from chronic illnesses to coping with difficult diagnoses - the voices of those affected paint a multifaceted picture of homeopathy, acupuncture and herbal medicine that fluctuates between skepticism and deep gratitude.
Many who turn to alternative approaches report a need for holistic care that they miss in conventional medicine. Anna, a 52-year-old woman with colon cancer, describes in an interview IllnessExperiences.de, how she resorted to herbal medicine alongside chemotherapy after her diagnosis. “I tried mistletoe preparations because I heard that they can strengthen the immune system,” she says. Although she didn't notice any measurable improvement in her tumor markers, she felt psychological support: "It made me feel like I was doing something for myself, not just waiting passively." Her experience reflects a commonly cited theme – the active role patients want to take in their recovery.
A similar search for control can be found in Manfred, who was diagnosed with solitary plasmacytoma in 2010 and later multiple myeloma. In a report Myeloma.org He describes how, after successful treatment, he used cannabis as an alternative method for pain. “The conventional painkillers had too many side effects,” he explains. “With cannabis I was able to sleep better and had fewer symptoms.” For him, this decision was not only a question of relief, but also of the quality of life, which he wanted to regain despite his serious illness. His words underline how alternative remedies are often used as a supplement to alleviate the burden of traditional therapies.
However, not all experiences are characterized by success. Sabine, who also suffers from multiple myeloma, tried homeopathy as an adjunctive therapy, but remained skeptical. “I took globules for nausea during chemo, but honestly, I didn't feel any difference,” she admits. Nevertheless, she valued the conversations with her homeopath, which offered her emotional support. This aspect - the interpersonal component - appears frequently in reports and shows that the perceived benefits of alternative methods often go beyond the physical effect and address psychological or social needs.
A mixed picture emerges when it comes to acupuncture. A 38-year-old patient with chronic back pain, quoted anonymously in an online forum, describes his first session as surprisingly pleasant: "I was afraid of the needles, but it was almost relaxing. After a few treatments I was able to move better." While he didn't experience a complete recovery, the method helped him reduce his pain medications. In contrast, another patient who tried acupuncture for migraines reported disappointing results: "I did six sessions, but the headaches came back just as often." These different experiences illustrate how individual reactions to such therapies can be.
A recurring theme in the stories is the desire for gentler alternatives, especially for serious illnesses such as cancer. Rita, who underwent high-dose chemotherapy with autologous stem cell transplant in 2017, turned to herbal supplements to combat side effects such as fatigue. “I took ashwagandha because it was recommended to me to regain energy,” she says. Although she has no scientific confirmation of the effect, she felt more energetic after a few weeks. Such reports show that subjective impressions often play a greater role than objective measurements, especially in moments when conventional medicine reaches its limits.
The social dimension of alternative healing methods is also often addressed. Andreas, who was diagnosed with bone marrow cancer in 2008, emphasizes how important it was to exchange ideas with other sufferers who tried similar methods such as acupuncture or herbal remedies. “You feel less alone when you hear that others are also looking for alternatives,” he reflects. For many, this community, often fostered through self-help groups, appears to be a crucial factor that increases the value of such approaches beyond their mere impact.
These personal insights shed light on the complex relationship between expectation, experience and actual benefits. While some patients find valuable support in alternative methods, others remain skeptical or disappointed. How these individual perspectives relate to the risks and rewards of such therapies opens the space for a final consideration of the balance between personal belief and scientific validation.
Regulatory aspects and guidelines
Navigating the labyrinth of healthcare often means dealing with a web of laws, regulations and cultural attitudes that shape access to alternative healing modalities. Globally, the legal framework for practices such as homeopathy, acupuncture and herbal medicine varies significantly, influencing both the availability and recognition of these approaches. From strict regulations to open integration into national health systems, the landscape is as diverse as the methods themselves, reflecting political, social and economic priorities.
In Germany, some alternative healing methods enjoy a comparatively high degree of acceptance and are partly integrated into the healthcare system. Phytotherapy, i.e. the use of medicinal plants, is officially regulated here, and many herbal medicines must be officially approved to ensure quality, effectiveness and safety. Acupuncture is covered by many health insurance companies for certain indications such as chronic pain, provided it is performed by qualified physicians. Homeopathy, on the other hand, is under greater scrutiny - although it is reimbursed by some health insurance companies as an additional service, there are ongoing debates about its funding through public funds as scientific evidence remains limited. These differences in recognition show how closely legal acceptance is linked to existing research Envivas described.
A look at Great Britain reveals a different dynamic. There, the National Health Service (NHS) has largely withdrawn support for homeopathy in recent years after extensive analyzes failed to provide convincing evidence of its effectiveness. Acupuncture, on the other hand, is offered by some NHS facilities in certain cases, such as pain management, although often with regional differences and under strict conditions. Herbal medicine is also subject to regulation by the Medicines and Healthcare products Regulatory Agency (MHRA), which ensures that herbal products are registered as traditional medicines if they meet certain safety and quality standards. This restrictive stance reflects a stronger orientation towards evidence-based medicine, which critically questions alternative approaches.
The United States presents a fragmented picture, characterized by a mix of government regulation and individual freedom. Acupuncture is recognized in many states and often requires practitioners to be licensed, although requirements vary by region. Some insurance plans, including Medicare, cover acupuncture for certain conditions such as chronic back pain, signaling its growing acceptance. Homeopathy and herbal medicine fall under the supervision of the Food and Drug Administration (FDA), but with less stringent regulations than conventional medicines - homeopathic products are often classified as dietary supplements and do not require prior approval, leading to concerns about safety and effectiveness. This loose regulation allows for broad access, but also poses risks for consumers.
A contrasting example is provided by India, where traditional systems such as Ayurveda are deeply rooted in the culture and supported by the state. The Ministry of AYUSH (Ayurveda, Yoga, Unani, Siddha and Homeopathy) oversees the training, research and practice of these methods, and many Ayurvedic treatments are available in public hospitals. Homeopathy also enjoys a strong position and is integrated into the national health system, with its own training centers and clinics. This institutional support contrasts with Western countries and shows how cultural values can shape legal recognition, even if scientific evidence for some practices remains limited.
In Switzerland, a significant step was taken in 2017 when certain alternative healing methods - including homeopathy, acupuncture and herbal medicine - were included in compulsory health insurance under certain conditions. This followed a referendum that called for greater integration of such approaches, but with the condition that their effectiveness, usefulness and cost-effectiveness be further examined. This development illustrates how political will and social pressure can influence the legal framework, even if the scientific community remains divided.
Global differences in regulation shed light on the complex interaction between tradition, public demand and scientific standards. While some countries see alternative healing methods as a valuable addition and support them through legal structures, others rely on stricter controls or exclude them from public systems. This diversity, influenced by political, social and economic factors, as on Technical word24 explains, shows that the recognition of such practices often depends less on their proven impact than on cultural and social contexts. The consequences this has for patients and healthcare systems opens up space for a final reflection on the balance between freedom and responsibility in medicine.
Criticism of alternative healing methods
There is often a deep gap between laboratory results and promises of healing, which scientists and doctors fill with sharp criticism of alternative healing methods. While homeopathy, acupuncture, and herbal medicine have gained adherents worldwide, they face significant resistance from the professional community, focusing on methodological weaknesses, lack of evidence, and potential risks. These concerns, raised by medical and research experts, shed critical light on practices that offer hope for many patients but often fail to meet rigorous standards for science.
A central accusation that runs through the criticism of all three methods is the lack of convincing scientific evidence. When it comes to homeopathy, experts particularly criticize the extreme dilutions, which often no longer contain detectable active ingredients. Many studies, including comprehensive meta-analyses, conclude that observed effects are mostly due to the placebo effect, as highlighted in numerous scientific discussions. Critics argue that the basic principles – such as the concept of “like cures like” – have no biochemical or physical basis, placing the method in the realm of pseudoscience. This reservation is reinforced by the fact that positive results in studies are often not reproducible or have methodological flaws, such as small samples or missing control groups.
There are similar reservations about acupuncture, although the evidence here is somewhat more differentiated. While some studies show positive effects on pain or nausea, scientists criticize the difficulty of distinguishing real from sham acupuncture in studies. Often, placebo treatments - in which needles are placed in non-specific points - produce comparable results, raising the question of whether the effect is specific or simply based on expectations. There is also criticism that many studies come from countries with a strong cultural influence of Traditional Chinese Medicine (TCM), which could lead to possible biases. These methodological challenges, as on Institute of Health explained, make it difficult to clearly assess the actual effectiveness.
When it comes to herbal medicine, including phytotherapy, the focus of criticism is the variability of the active ingredients and the inadequate standardization. Doctors point out that the concentration of active ingredients in herbal preparations depends heavily on factors such as climate, harvest time or processing, which makes the reproducibility of study results difficult. While some plants such as St. John's wort for depression or turmeric for inflammation provide promising data, long-term studies proving sustainability and safety are often lacking. There are also criticisms that many studies include small groups of test subjects and use subjective reports instead of objective measurement instruments, which reduces their informative value. Another point is the risk of interactions with conventional medications, which is often underestimated.
Beyond the evidence, scientists raise concerns about patient safety. A frequently cited point of criticism is that alternative healing methods are sometimes used as a replacement for proven therapies, which can have fatal consequences in serious illnesses such as cancer. Doctors warn that delaying or foregoing evidence-based treatments in favor of unproven approaches increases the risk of disease progression. This concern is particularly true in homeopathy, where the absence of pharmacologically active substances in many preparations means that no specific medicinal effect can be expected. Herbal medicine also raises concerns about potential toxicity or allergic reactions, which can be aggravated by unregulated products.
Another point of contention is the role of industry and marketing, which, according to critics, often spreads exaggerated promises of healing. Scientists complain that many alternative products and services are promoted using anecdotal reports or pseudoscientific explanations, without independent research to support the claims. This is particularly true in homeopathy and some herbal preparations, where commercial interests can distort perceptions of effectiveness. There are similar reservations with less researched methods such as healing stones, where critics like on Star paths presented, emphasize that the industry often benefits more from belief than evidence.
Finally, the ethical dimension is often addressed, particularly the question of patient information. Doctors are demanding that providers of alternative healing methods be obliged to provide clear information about the limits and risks of their approaches. Without this transparency, patients could develop unrealistic expectations, which undermines trust in all medicine. These criticisms, ranging from methodological weaknesses to safety concerns, highlight the tension between individual choice and collective responsibility in health care. How these concerns impact the future of alternative healing modalities opens space for a final consideration of the balance between innovation and evidence.
Future of alternative healing methods

Let us imagine a future in which the boundaries between ancient wisdom and modern science no longer separate but connect - a horizon where alternative healing modalities such as homeopathy, acupuncture and herbal medicine could redefine their place in healthcare. The development and integration of these approaches into modern medicine is at a turning point, driven by growing demand, technological advances and an increasing pursuit of holistic care. This outlook highlights possible paths that these practices could take and the challenges that need to be overcome to achieve harmonious coexistence with evidence-based medicine.
One promising trend is the growing acceptance of integrative medicine, which combines alternative and conventional approaches to achieve the best of both worlds. Institutions like the Cleveland Clinic have already established programs that incorporate methods such as acupuncture, Chinese herbal therapy and yoga into their treatment plans to relieve conditions such as chronic pain, indigestion or menopausal symptoms Cleveland Clinic described. This integrative approach aims to not only treat symptoms but also promote overall well-being by combining patient wishes and clinical expertise. Such models could become more important in the coming years as they build a bridge between tradition and modern research.
In parallel, there is a notable increase in the popularity of complementary practices, particularly psychological and physical approaches. Data from the National Health Interview Survey (NHIS) illustrates this shift: Between 2012 and 2017, the practice of yoga increased from 9.5% to 14.3% and that of meditation increased from 4.1% to 14.2% among U.S. adults, as on NCCIH documented. This trend reflects a growing interest in stress-reducing and preventative measures that are easily accessible and can often be carried out without medical supervision. Increasing demand could lead to greater integration of such methods into public health programs, particularly to support chronic illness or mental health.
Another driver for the development of alternative healing methods is ongoing research aimed at better understanding their mechanisms and effects. For acupuncture, for example, there are already numerous studies that demonstrate specific benefits for pain or migraines, and future studies could provide even more precise results through improved study designs and larger groups of test subjects. The same applies to herbal medicine, where standardization of extracts and conducting long-term studies are crucial to ensure safety and effectiveness. Even for controversial approaches such as homeopathy, new approaches to placebo research could shed light on the psychological components of healing. In the long term, this scientific curiosity could help separate the wheat from the chaff and formulate well-founded recommendations.
Technological innovations also offer exciting prospects for the integration of alternative methods. Digital platforms and apps that offer personalized yoga or meditation programs make such practices accessible to a wider audience and could be customized through AI-powered analytics to achieve maximum benefits. Likewise, telemedicine services could facilitate consultations on herbal therapies or acupuncture by connecting patients with certified practitioners, regardless of geographic barriers. These developments could significantly expand the reach of alternative approaches while improving the quality of care through standardized protocols.
At the same time, however, there are hurdles in the way that make seamless integration difficult. Skepticism from the scientific community, coupled with regulatory challenges, means that many alternative methods continue to struggle for recognition. Funding for research remains a critical issue – without sufficient funding, promising approaches such as integrative therapies or specific herbal preparations may not receive the necessary evidence base to be incorporated into healthcare systems. In addition, training medical professionals in these areas requires interdisciplinary efforts to reduce prejudices and promote constructive dialogue.
The future of alternative healing methods could also be shaped by social and cultural changes that increase the focus on prevention and self-care. As demand for personalized and holistic approaches grows, healthcare systems may be forced to develop more flexible models that are more responsive to patient preferences. The role homeopathy, acupuncture and herbal medicine play in this change depends on how well they can adapt to the demands of evidence-based medicine without losing their unique perspective. This balance between tradition and innovation opens the space for a final reflection on the possibilities and limits of an integrative healthcare system.
Sources
- https://www.envivas.de/magazin/gesundheitswissen/alternative-heilmethoden
- https://de.wikipedia.org/wiki/Alternativmedizin
- https://en.wikipedia.org/wiki/Homeopathy
- https://www.nccih.nih.gov/health/homeopathy
- https://en.m.wikipedia.org/wiki/Homeopathy
- https://www.mayoclinic.org/tests-procedures/acupuncture/about/pac-20392763
- https://en.m.wikipedia.org/wiki/Acupuncture
- https://pmc.ncbi.nlm.nih.gov/articles/PMC8868048/
- https://www.tcm.edu/news/detail/news/neue-evidenz-zur-wirksamkeit-der-akupunktur-open-access-studie-veroeffentlicht
- https://natur.wiki/gesundheit-ernaehrung/kraeutermedizin-heilkraeuter-und-ihre-anwendungen
- https://www.susannekaiser.com/%C3%BCber/kr%C3%A4utermedizin/
- https://www.eingepflanzt.de/die-wissenschaft-der-kraeuter-eine-studie-ueber-heilkraeuter/
- https://scisimple.com/de/articles/2025-06-09-kraeutermedizin-im-aufstieg-gegen-medikamentenresistente-bakterien–ak4ojd8
- https://unterschied.de/unterschied-zwischen-akupunktur-und-homoeopathie/
- https://de.wikipedia.org/wiki/Pflanzenheilkunde
- http://www.krankheitserfahrungen.de/module/darmkrebs
- https://www.myelom.org/shgs-links/erfahrungsberichte.html
- https://fachwort24.com/was-sind-rahmenbedingungen-aufklaerung-beispiele-xz2/
- https://sternenpfade.com/heilsteine-wissenschaftliche-kritik
- https://institut-der-gesundheit.com/gesundheit-ernaehrung/evidenzbasierte-naturheilkunde-kritische-betrachtung-aktueller-forschung
- https://my.clevelandclinic.org/health/treatments/21683-integrative-medicine
- https://www.nccih.nih.gov/health/complementary-alternative-or-integrative-health-whats-in-a-name
- https://www.gesundheit.com/gesundheit/alternative-medizin/1/alternative-heilmethoden-ganzheitliche-ansaetze-nutzen-und-risiken-im-berblick
- https://www.magazin-welt.com/alternative-heilmethoden-wirksamkeit-risiken-der-weg-zu-mehr-wohlbefinden/

 Suche
Suche
 Mein Konto
Mein Konto
