With the help of cells instead of tablets, many diseases could be detected, prevented and cured: the future of medical therapy.
Leveraging competent bacteria A new study published today in Science describes how scientists genetically modified bacteria to successfully detect cancer cells. This breakthrough could help improve cancer diagnosis and potentially enable targeted biological therapies in the future. The project began with a talk by synthetic biologist Rob Cooper during a weekly lab meeting at the University of California, San Diego. Cooper worked on the study of genes and gene transfer in bacteria. Genes are the basic units of genetic inheritance. Among other things, they determine the characteristics that we inherit from our parents. During gene transfer...
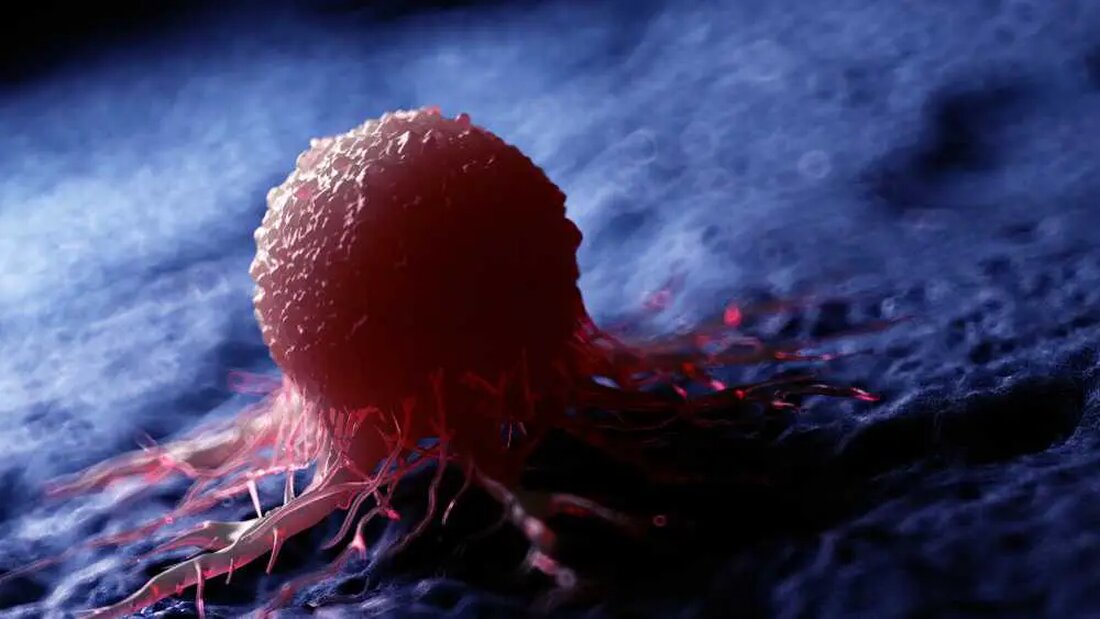
With the help of cells instead of tablets, many diseases could be detected, prevented and cured: the future of medical therapy.
Leveraging competent bacteria
A new study published today in Science describes how scientists genetically modified bacteria to successfully detect cancer cells. This breakthrough could help improve cancer diagnosis and potentially enable targeted biological therapies in the future.
The project began with a talk by synthetic biologist Rob Cooper during a weekly lab meeting at the University of California, San Diego. Cooper worked on the study of genes and gene transfer in bacteria.
Genes are the basic units of genetic inheritance. Among other things, they determine the characteristics that we inherit from our parents. Gene transfer involves transferring genes from one cell to another. This can occur vertically, when a cell divides and replicates its DNA, or horizontally, when DNA is exchanged between unrelated cells.
Horizontal gene transfer is widespread in the microbial world. Certain bacteria can absorb genes from the free DNA in their immediate environment. This happens when cells die and their DNA is released. Bacteria can absorb this free DNA into their own cells and use it to adapt evolutionarily.
This process allows bacteria to explore their environment and pick up genes that could give them an advantage. The idea behind genetically modifying bacteria to detect cancer is based on the fact that cancer is defined by changes in the genetic material of cells.
The researchers chose the bacterium Acinetobacter baylyi as an experimental biosensor to detect diseases. The A. baylyi genome was modified to contain long DNA sequences similar to the human cancer gene they wanted to capture. These “complementary” DNA sequences acted as adhesive surfaces where the specific tumor genome DNA could be integrated into the bacterial genome.
An important goal was to keep the tumor genome DNA in the bacterium in order to activate other genes. In this case, it was an antibiotic resistance gene that was used as a signal to detect cancer. If the bacteria were able to grow on antibiotic culture plates, their antibiotic resistance gene was active and this indicated cancer detection.
The team conducted a series of experiments introducing the new bacterial biosensor and tumor cells into increasingly complex systems. First, the bacteria were treated with purified tumor genomic DNA and the biosensor successfully detected the tumor genomic DNA.
The bacteria were then cultured together with living tumor cells and the tumor genome DNA could also be recognized here. Finally, the bacteria were injected into live mice, which either had tumors or didn't. In a mouse model of colon cancer, the biosensors were able to reliably distinguish between mice with and without colon cancer.
Following these promising results, the bacterial biosensor was further improved and can now distinguish individual base pair changes within the tumor genomic DNA. This technology, called CATCH (Cellular Assay for Targeted, CRISPR-Discriminated Horizontal Gene Transfer), has great potential and could be used in the future to detect a variety of diseases, particularly infections and cancer.
However, the technology is not yet ready for use in the clinic. The researchers are actively working on further development to improve the efficiency of DNA detection and to critically evaluate the performance of the biosensor in comparison to other diagnostic tests. In addition, the safety of patients and the environment must be guaranteed.
However, perhaps the most exciting prospect of cellular medicine is not just disease detection. Biosensors could be programmed so that when a specific sequence of DNA is detected, they can trigger a specific biological therapy directly at the site where the disease is detected in real time.
The development of this innovative technology is the result of successful collaboration between various scientists and researchers. The team included Professor Jeff Hasty, Dr. Rob Cooper, Associate Professor Susan Woods and Dr. Josephine Wright.
The results of this study are promising, but further testing is required to validate the performance of the biosensor and explore its potential application in clinical practice. However, the future of cellular medicine looks promising and could lead to revolutionary changes in the diagnosis and treatment of disease.
This article was republished from The Conversation under a Creative Commons license.

 Suche
Suche
 Mein Konto
Mein Konto
