Relation
Wallen ZD, Appah M, Dean Mn, et al. Characteristic dysbiosis of the intestinal microbioma at PD: Evidence of an over -unimination of opportunistic pathogens.NPJ Parkinsons Dis. 2020;6:11.
Draft
A case control study on intestinal microbiom-wide associations of people with Parkinson's disease (PD) compared to neuro-healthy checks.
Participant
Two data sets were presented in the study. Dataset 1 included 197 Parkinson's cases and 130 neurohealthy controls with participants from Albany, New York, Seattle, Washington, and Atlanta, Georgia. Dataset 2 included 323 Parkinson's cases and 184 neurohealthy controls from Birmingham, Alabama.
Primary outcome measures
The primary result of this study was the abundance of gastrointestinal microbes and patterns at the same time.
The researchers analyzed all data with and without disruptive factors, including geography, gender, age, constipation in the past 3 months, gastrointestinal complaints, daily fruit and vegetable consumption, body mass index (BMI), alcohol consumption, weight loss and Parkinson's medication.
Key insights
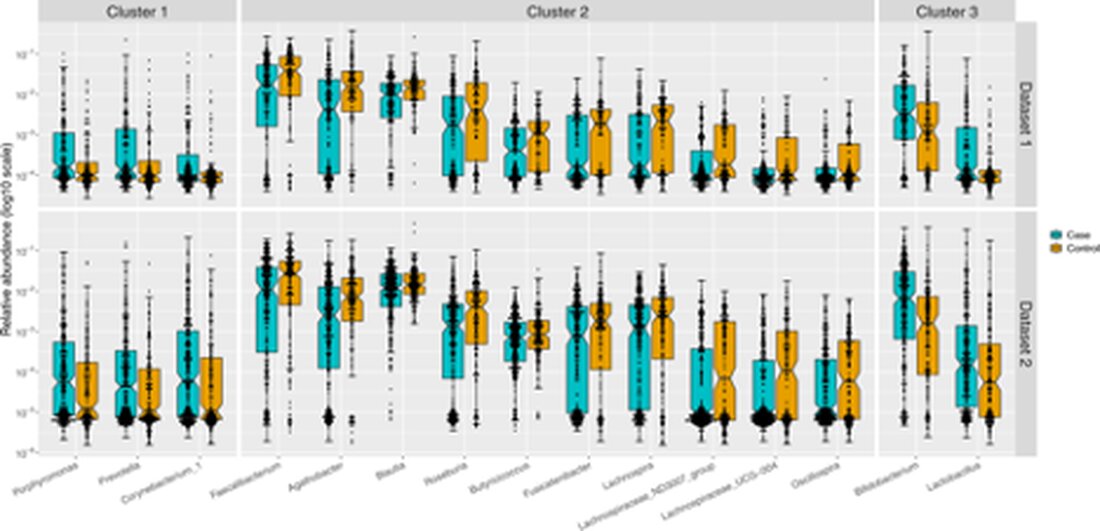
The researchers discovered 3 clusters, which included 15 different genera in people with Parkinson's, but not with neuro -healthy control persons, which indicates that these microbes are associated with Parkinson's.
Cluster 1: Those with PD had a wealth ofPorphyromonas,PrevotellaandCorynebacterium_1 generacompared to controls. Although these microbes are in normal numbers, if they are overgrown in the intestine, they can contribute to the progress of the disease. The authors suggest that the microbes increased at PD could act as opportunistic pathogens.
Cluster 2 contained 10 genera that were present at lower frequencies in the 2 cohorts of participants with PD compared to controls. The majority of genera in cluster 2 were anaerobic, gram-positive bacteria in theRuminococcaceaeandLachnospiraceaeFamilies who are known to produce butyrat and other short -chain fatty acids in the intestine.
Cluster 3 is the strangest. Although those with PD do not take probiotic nutritional supplements, they had a higher abundanceLactobacilliandBifidobacteriaSpp.
"The relative frequencies in PD cases (blue) and controls (orange) were applied as a log10 scale on the y-axis. The sample size was 201 cases and 132 checks in data record 1 and 323 cases and 184 controls in data record 2. Each point represents a sample according to the relative frequency of the genus. Confidence of the Median. Extend mustache hairs are outliers. " Reprint under Creative Commons 4.0 license.
Practice implications
Intestinal dysgosis increasingly occurs in Parkinson's disease.1-3While it is tempting to focus on the brain when dealing with a neurological disease, it is clear that the gut influences the course of the disease.1From a clinical perspective, this study suggests that physicians should address the gut along with the brain in their patients with Parkinson's disease.
What inhabits the gut and forms the microbiome is primarily influenced by diet. Prebiotics, such as those found in fruits, vegetables, mushrooms and legumes, lead to increased production of butyrate, an anti-inflammatory short-chain fatty acid (SFCA). Gut microbes ferment indigestible oligosaccharides, including onions, leeks, asparagus, artichokes, and beets, to produce butyrate.4sugar alcohols, such as polyols from fruits,5and some proteins may also support butyrate production. However, endogenous butyrate production depends on the right microbial species to ferment the fibers, and this study showed that these SCFA-producing microbes are deficient in people with Parkinson's disease (cluster 2).
A strategy to increase butrate includes increasing the amount of fruit and vegetables in the nutrition of people with Parkinson's. In fact, research results indicate that a Mediterranean diet can reduce the risk of Parkinson's Parkinson's or delay the outbreak of the disease.6-9Regardless, a ketogenic diet can increase hydroxybutyrate, and 2 small studies suggest that some people with Parkinson's (but not all) respond well to a ketogenic diet.10.11It is also possible that some people with Parkinson's need additional butyrat because only a few SCFA-producing bacteria colonize their large intestine; However, this remains speculative because there are no studies that confirm this presumption.
The increased number ofBifidobacteriumandLactobacilliindicate that the administration of these special probiotics in people with Parkinson's is not indicated and that the amount of Levodopa medication can actually affect that is required to control symptoms.
Another strategy for increasing butyrate is to prescribe probiotics that contain butyrate-producing microbes. However, over-the-counter probiotics usually do not contain anyLactobacilliSPP andBifidobacteriumSPP, both of whom were more likely to have occurred in the current study in patients with PD. Usually your presence is associated with a cheaper environment for the thrive of the butyrat-producing bacteria. The authors claim that the high occurrence of these popular probiotics could be due to the use of PD medication, including Levodopa. In fact,Lactobacillispp convert levodopa into dopamine, so it can be considered the energy substrate of this genus. The more levodopa/carbidopa a person takes, the moreLactobacilliSPP grow to metabolize it, which then requires the administration of ever higher amounts of Levodopa/Carbidopa. The intake of plants and dairy products can also increaseLactobacilliandBifidobacteriumspp. Alternatively thisLactobacilliandBifidobacteriumCould be compensatory if the intestine increases its frequency to counteract the less SCFA-producing species that occur in the intestine of patients with PD.
The increased number ofBifidobacteriumandLactobacillisuggest that administration of these specific probiotics is not indicated in people with Parkinson's disease and may actually affect the amount of levodopa medication needed for symptom control. However, there is a previous study showing that probiotics (found in fermented milk) can reduce constipation in people with Parkinson's12- maybe because increasedLactobacilliincreases dopamine that is responsible for intestinal contraction. Regardless of this, the administration of probiotics must be carefully weighed in these patients.
Several recent research studies have shown the effects of non -antibiotic medicines on the microbioma.13.14This study confirms these results at PD. While PD medication did not affect the excessive growth of pathogenic microbes, these drugs may have reduced the SCFA-producing microbes and theBifidobacteriumandLactobacillispp.As a clinician, it is important to recognize that all medicines and herbs have microbiomic relationships that must be taken into account. As we learn how dysbiosis plays a role in Parkinson's disease, clinicians should be prepared to change their long-held beliefs about what is useful or potentially harmful in their approach to dysbiosis in this population.

 Suche
Suche
 Mein Konto
Mein Konto