A aggressive blood cancer, which primarily affects children, has 15 different subtypes, each associated with a specific outcome and response to medication, according to a genomic analysis 1. The work promises to improve treatment — for example, sparing some children from the harshest chemotherapy regimens and giving others the latest immunotherapies.
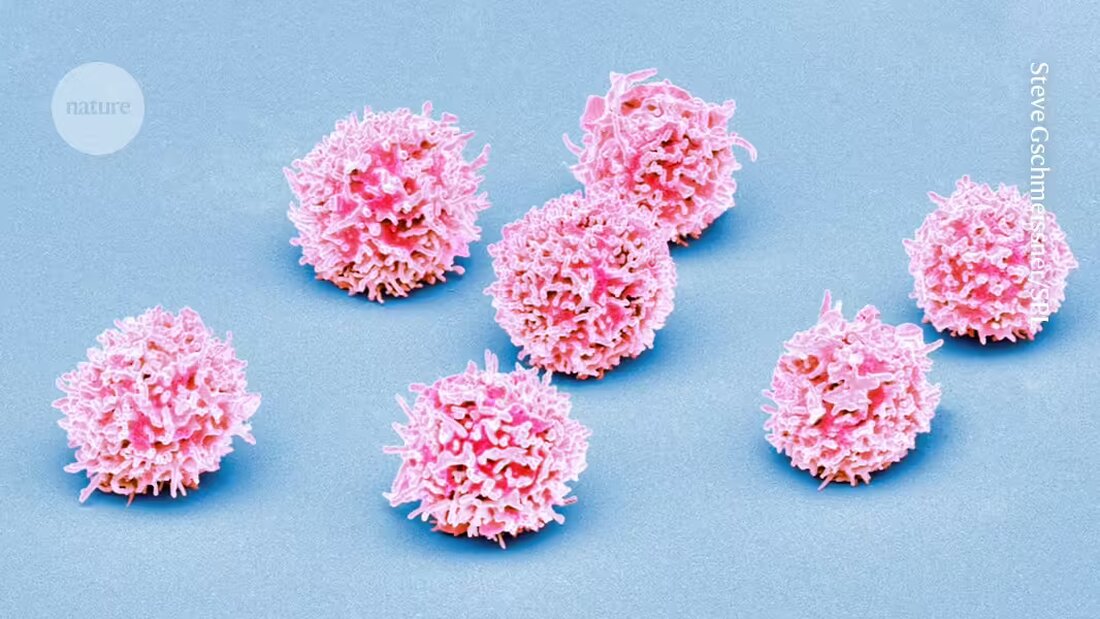
This detailed classification paves the way for targeted therapies, researchers say, and offers people with T cell acute lymphoblastic leukemia (T-ALL) Hope, which accounts for approximately 5% of all pediatric cancers. The ones in todayNaturePublished work could help predict who is less likely to respond to treatment and help doctors choose more effective therapies from the start.
“It's a great study that will be a very rich resource for anyone treating T-ALL patients,” says Jan Cools, a leukemia genetics researcher at the Flemish Institute of Biotechnology in Ghent, Belgium, who was not involved in the research.
A degenerated stem cell
T-ALL occurs when a mutated stem cell in the bone marrow produces large amounts of abnormal T cells, a type of immune cell. Although survival rates for T-ALL have improved with advances in chemotherapy, 15-20% of children and teenagers experience relapses or have forms of the disease that do not respond to standard treatment, according to study co-author David Teachey, a pediatric oncologist and researcher at the Children's Hospital of Philadelphia in Pennsylvania. Therefore, it is important to find better biological markers that can predict which people with T-ALL need targeted therapies or new treatment approaches.
Previously, research had identified different subtypes of T-ALL, but no study was large enough to reliably predict a person's disease progression based on genetic changes alone. So Teachey and his colleagues analyzed the entire DNA sequence of both tumor cells and healthy cells from more than 1,300 people with T-ALL who received the same treatment. The researchers also examined cellular RNA to understand how gene activity was altered in the cancer samples.
Linking genome and outcome
The analysis revealed 15 different T-ALL subtypes, some previously uncharacterized. Each subtype showed unique genetic alterations and gene expression patterns. People with certain subtypes were more likely to have cancer cells remaining in the body after treatment, which can lead to a relapse of the disease. People with other subtypes were more likely to survive and remain cancer-free, and one subtype was more likely to lead to another type of cancer elsewhere in the body, the researchers found.
The analysis also showed that almost 60% of the genetic changes associated with T-ALL DNA sections occur that do not produce proteins but can influence gene activity. These changes often led to inappropriate activation of genes and contributed to cancer development.
Using genetic and clinical data, researchers classified T-ALL by risk level: very high, high, low and very low. This classification could help doctors tailor treatments by recommending stronger chemotherapy or new immunotherapies for high-risk people and less aggressive treatments for those at lower risk, Cools says.
The study attracted participants from the United States, Canada, Australia, Switzerland and New Zealand. Because a person's genetic history can influence their response to treatment, the results need to be validated in different populations, says study co-author Charles Mullighan, a hematologist at St. Jude Children's Research Hospital in Memphis, Tennessee.
The research also highlights the need to analyze the entire DNA sequence of tumor cells in people with T-ALL. Although this 'whole genome sequencing' is not yet widely used due to its cost, Mullighan expects it to become more common in the future. “Studies like this make a compelling case that we should increasingly pursue whole-genome sequencing for this type of leukemia.”

 Suche
Suche
 Mein Konto
Mein Konto