As the World Health Organization (WHO) declared a public health emergency over Mpox earlier this month It was because a worrying form of the virus that causes the disease had spread to several African countries where it had never been seen before. Since then, two people traveling to Africa — one from Sweden and one from Thailand — have become infected with this clade 1b virus and brought it back to their countries.
Although researchers have known about the current outbreak since late last year, the need for answers is now more urgent than ever. The Democratic Republic of Congo (DRC) in Central Africa has been battling the Clade I virus — a group that includes Ib — for decades. So far, Clade I infections usually arise when a person has contact with wild animals, and outbreaks stall.
Clade Ib appears to be different and spreads primarily through human contact, including through sex. In the DRC alone, nearly 18,000 cases of Mpox — many of them in children — and at least 600 deaths have been reported this year.
How does this emergency compare to the one declared in 2022 when Mpox cases emerged worldwide? How does this virus compare to the version that caused this outbreak, a species called Clade II? And will Africa manage to get this problem under control?Naturetalks to researchers about the information they're rushing to collect.
Is Clade Ib deadlier than the other virus types?
It's hard to determine, says Jason Kindrachuk, a virologist at the University of Manitoba in Winnipeg, Canada. There are currently two simultaneous outbreaks in the DRC. The Clade I virus, which has been endemic in forested regions of the DRC for decades, is circulating in rural areas where people get it from animals. This clade was renamed Ia after the discovery of clade Ib. Animal studies suggest that Clade I is deadlier than Clade II 1, but Kindrachuk says it's difficult to speculate what that means for people.
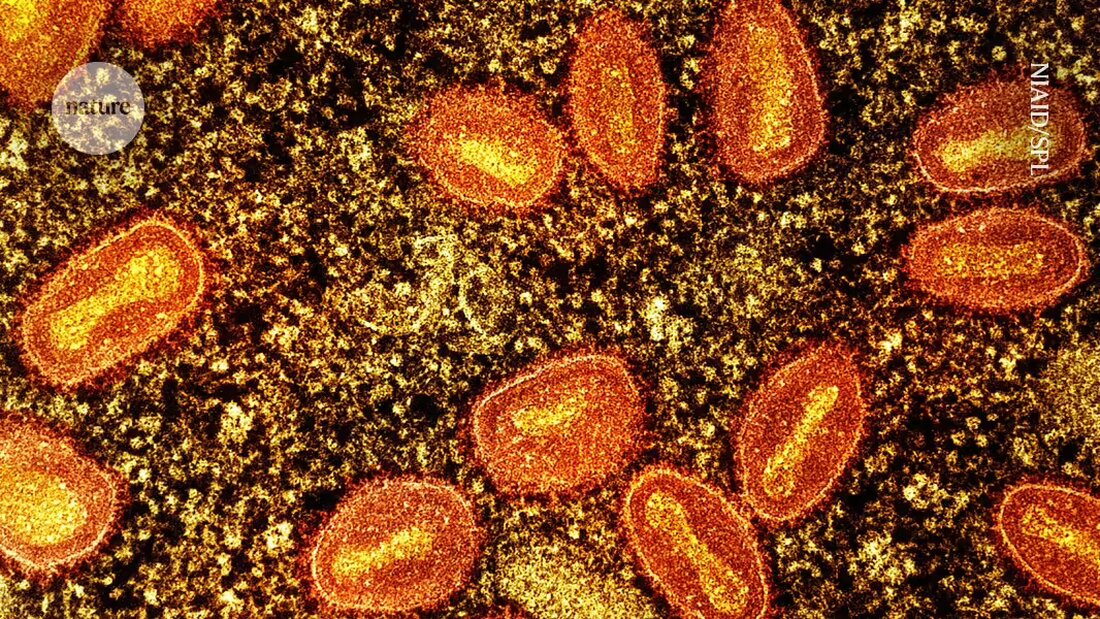
Even if not fatal, Mpox can cause fever, aches, and painful, fluid-filled skin lesions.
Although many reports say that 10% of Clade I infections in humans are fatal, infectious disease specialist Laurens Liesenborghs at the Institute of Tropical Medicine in Antwerp, Belgium, doubts that number is accurate. Even the WHO's latest estimate of a 3.5% mortality rate among people with Mpox in the DRC may be high.
There are many reasons why mortality estimates could be unreliable, says Liesenborghs. On the one hand, the surveillance data only records the most serious cases. Many people who are less sick may not seek treatment in hospitals or from doctors, so their infections go unreported.
Another factor that can distort the mortality rate is a secondary health disorder. For example, people with HIV — who make up a significant proportion of the population in many African countries — die from Mpox at a rate twice as high as people who do not have compromised immune systems, especially if their HIV is untreated 2. The high death rate among children under 5 may be due in part to malnutrition, which is common among children in rural parts of the DRC, says Liesenborghs.
Is Clade Ib more contagious than other types?
The clade 1b virus has attracted particular attention because epidemiological data suggests that it transmits more easily between humans than previous strains, including through sexual activity, while clade Ia originates primarily from animals. An analysis published last week ahead of peer review on the preprint server medRxiv 3, shows that the genome of clade Ib contains genetic mutations that appear to have been induced by the human immune system, suggesting that it has existed in humans for some time. Clade Ia genomes have fewer of these mutations.
But Liesenborghs says the mutations and clades may not be the most important factor in understanding how the monkeypox virus spreads. Although it is useful to distinguish Ia from Ib, he says, the severity and transmissibility of the disease may be more influenced by the region in which the virus is circulating and the people living there. For example, Clade Ia appears to be more common in sparsely populated rural regions where it is less likely to spread widely. Clade Ib appears in densely populated areas and spreads more quickly.
Jean Nachega, an infectious disease doctor at the University of Pittsburgh in Pennsylvania, says scientists don't understand many aspects of Mpox transmission — they haven't even figured out which animal serves as a reservoir for the virus in nature, although rodents can carry it. “We have to be very humble,” says Nachega.
How effective are vaccines against the Clade I virus?
As was the case during the COVID-19 pandemic, health experts are looking to vaccines to contain the current Mpox outbreak. Although there are no vaccines specifically designed to combat the monkeypox virus, there are vaccines that have helped ward off a related virus — the one that causes smallpox. Two currently exist. Jynneos, made by Bavarian Nordic in Hellerup, Denmark, contains a type of smallpox virus that cannot reproduce but can trigger an immune reaction. LC16m8, manufactured by KM Biologics in Kumamoto, Japan, contains a live — but weakened — version of a different strain of smallpox virus.
However, it is unclear how effective these smallpox vaccines generally are against Mpox. Dimie Ogoina, an infectious disease specialist at Niger Delta University in Wilberforce Island, Nigeria, points out that vaccines have only been tested against the Clade II virus in European and American populations, as these vaccinations distributed by wealthy countries during the global outbreak that began in 2022. And the recipients were mostly young, healthy men who have sex with men, the population that drove this outbreak. A study in the United States found that one dose of Jynneos was 80% effective in people at risk, while two doses were 82% effective 4; the WHO recommends receiving both vaccinations.
People in Africa infected with the clade Ia or 1b virus — particularly children and those with compromised immune systems — may react differently, although a study in the DRC found that the Jynneos vaccine was generally able to produce antibodies against Mpox in about 1,000 health workers.
But researchers are trying to fill some data gaps. A team in the DRC will soon start a clinical trial of Jynneos in people who have come into close contact with the monkeypox virus — but have not shown symptoms — to see whether it can prevent future infection or improve outcomes.
Will the vaccines help contain the latest outbreak?
Until now, Mpox vaccines have been largely unavailable in Africa, but several wealthy countries have pledged to donate doses to the DRC and other affected African countries. The United States has offered 50,000 Jynneos doses from its national stockpile and the European Union has ordered 175,000, with individual member countries pledging additional doses and Bavarian Nordic adding another 40,000. Japan has offered 3.5 million doses of LC16m8 (which requires just one shot instead of two).
None of these doses have arrived so far, says Espoir Bwenge Malembaka, an epidemiologist at the Catholic University of Bukavu in the DRC. Low- and middle-income countries that rely on vaccine donations will not be able to receive them until WHO confirms the shots are safe and effective. The WHO has not yet given the green light. It is assessing additional data it received from vaccine manufacturers that prevents shippers from sending the vaccines.
Even if the vaccines arrive, Bwenge Malembaka says, “it’s really a drop in the ocean.” The African Centers for Disease Control and Prevention in Addis Ababa, Ethiopia, estimates that 10 million doses will be needed to contain the outbreak.
Bwenge Malembaka says uncertainty over vaccine delivery has made it difficult for the government to come up with a distribution plan. “I don’t know how to address this problem,” he says. Bwenge Malembaka suspects children are likely to receive doses first because they are particularly vulnerable to Clade I, but authorities have not yet decided which regions to target. It is also unclear how the government would prioritize other vulnerable populations, such as: B. Sex workers affected by clade Ib. Their profession is criminalized in the DRC, so they may not be able to report for treatment.
Researchers regret that public health organizations did not provide vaccines and other resources early when the Clade I outbreak was identified, especially given the lessons learned from the 2022 global Mpox outbreak. "The opportunity existed a few months ago to break this chain of transmission, but the resources were not available," says Liesenborghs. “Now it will be more difficult to manage this outbreak and the population at risk is much broader.”

 Suche
Suche
 Mein Konto
Mein Konto