Hidden Diagnosis: Colitis in Familial Mediterranean Fever - Crohn's Disease or Ulcerative Colitis?
A 24-year-old woman with familial Mediterranean fever presents with alternating intestinal inflammation resembling Crohn's or ulcerative colitis. Gene variants discovered, colchicine led to remission.
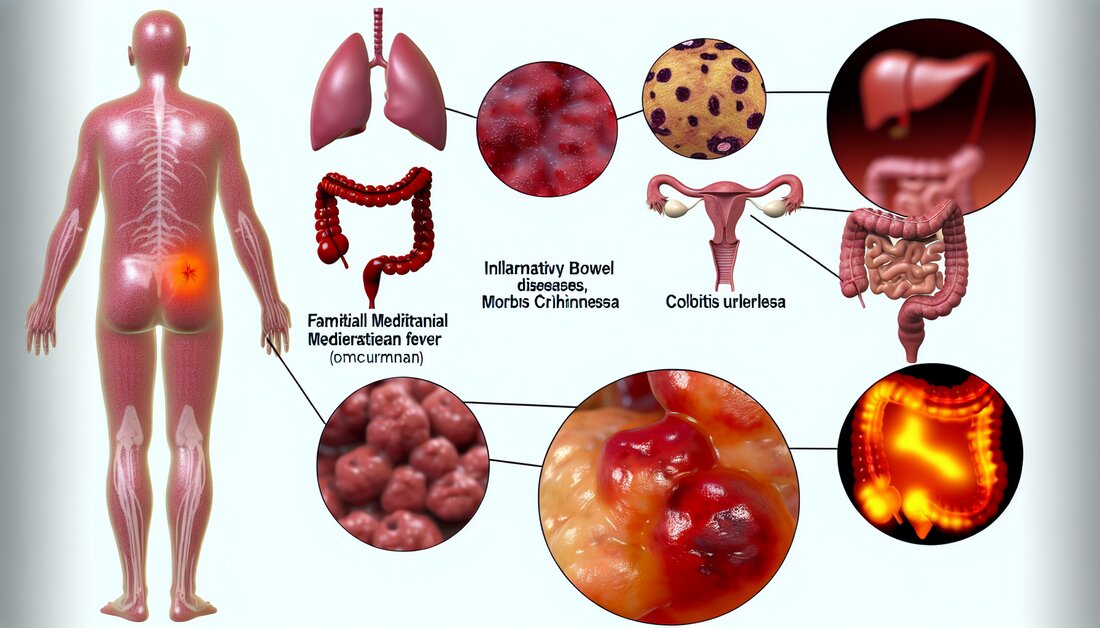
Hidden Diagnosis: Colitis in Familial Mediterranean Fever - Crohn's Disease or Ulcerative Colitis?
The research presented here describes an interesting case of a young woman who suffered from abdominal pain, fever and joint pain. At first everything seemed to indicate that she was suffering from the chronic intestinal disease Crohn's disease, but the usual treatments failed. It was only after doctors changed her diagnosis and conducted genetic testing that they discovered her symptoms were due to a rarer condition, familial Mediterranean fever (FMF). Simple therapy with the drug colchicine then led to complete improvement.
In the future, this discovery could mean that doctors could consider genetic testing and therapy with colchicine as a possible option for unusual and changing intestinal diseases, especially if conventional treatment approaches do not provide any improvement.
Basics and terms
Crohn's disease:A chronic inflammation of the intestine that occurs in episodes and is often accompanied by abdominal pain, diarrhea and weight loss. Diagnosis is typically made through a colonoscopy.
Ulcerative colitis:Another chronic intestinal disease that differs from Crohn's disease in its continuous development and the different patterns of infection in the intestine. Inflammation usually occurs continuously in the large intestine.
Familial Mediterranean Fever (FMF):A genetic disease commonly found in Mediterranean countries. It is characterized by recurring episodes of fever and inflammation, usually in the abdomen, joints or chest.
Colchicine:A drug commonly used to treat gout and FMF. It works by reducing the inflammatory response in the body.
Abbreviations
- FMF: Familiäres Mittelmeerfieber
- Koloskopie: Untersuchung des Dickdarms mit einer Kamera
Changes in colonic inflammation as an indicator of familial Mediterranean fever-associated enterocolitis
In a recent study, a 24-year-old female patient with symptoms initially suggestive of Crohn's disease was examined. The treatment approaches implemented, including 5-aminosalicylic acid, azathioprine and infliximab, were without clinical success. A later colonoscopy revealed a picture more consistent with active ulcerative colitis. These observations led to a genetic study that revealed variants of the MEFV gene.
Genetic discoveries and treatment successes
The patient was found to carry the MEFV gene variants E148Q and L110P in exon 2. These variations are known in scientific circles to be associated with familial Mediterranean fever (FMF). Treatment with colchicine resulted in complete clinical remission, supporting the hypothesis that the observed changes in colonic inflammation may indicate FMF-associated enterocolitis.
Significance of clinical observations
- Langfristige Veränderungen von Kolonläsionen können als diagnostische Hinweise für FMF-assoziierte Enterokolitis dienen.
- Unterschiedliche morphologische Merkmale im Krankheitsverlauf, wie der Wechsel von einem Crohn-ähnlichen zu einem Colitis ulcerosa-ähnlichen Erscheinungsbild, sind von entscheidender Bedeutung.
- Genetische Tests spielen eine wesentliche Rolle bei der Bestätigung und Anpassung der Diagnose.
- Colchicin hat sich in diesem Fall als wirkungsvolle Behandlung erwiesen.
Table: Main features and diagnostic developments
| Investigation | Result | Treatment |
|---|---|---|
| Colonoscopy (initial examination) | Elongated ulcers, cobblestone-like appearance | 5-aminosalicylic acid, azathioprine, infliximab (no remission) |
| Colonoscopy (follow-up examination) | Diffuse granular mucosa, active ulcerative colitis | Genetic testing |
| Genetic diagnostics | Variants E148Q, L110P in exon 2 | Colchicine (full remission) |
These findings demonstrate that genetic factors are crucial for correct diagnosis and treatment and that morphological changes can provide crucial clues to the underlying pathology. Further research will be necessary to unlock the full diagnostic potential of these observations.
For full details of the study please visit the external link: https://pubmed.ncbi.nlm.nih.gov/39295638.

 Suche
Suche
 Mein Konto
Mein Konto
