Harness the healing power of smart” stem cells from human fat
Smart Stem Cells Discovered from Human Adipose Tissue: A Breakthrough in Regenerative Medicine Researchers have recently discovered a new type of smart stem cell known as induced multipotent stem cells (iMS). This discovery represents a significant advance in the field of regenerative medicine. iMS cells are derived from human adipose tissue and have demonstrated their impressive ability to adapt and transform in animal studies, demonstrating their potential for tissue repair. Professor John Pimanda from UNSW Medicine & Health explains that iMS cells are unique in their ability to respond to their environment. The fact that stem cells are able to respond to their environment and...
Harness the healing power of smart” stem cells from human fat
Intelligent stem cells discovered from human adipose tissue: A breakthrough in regenerative medicine
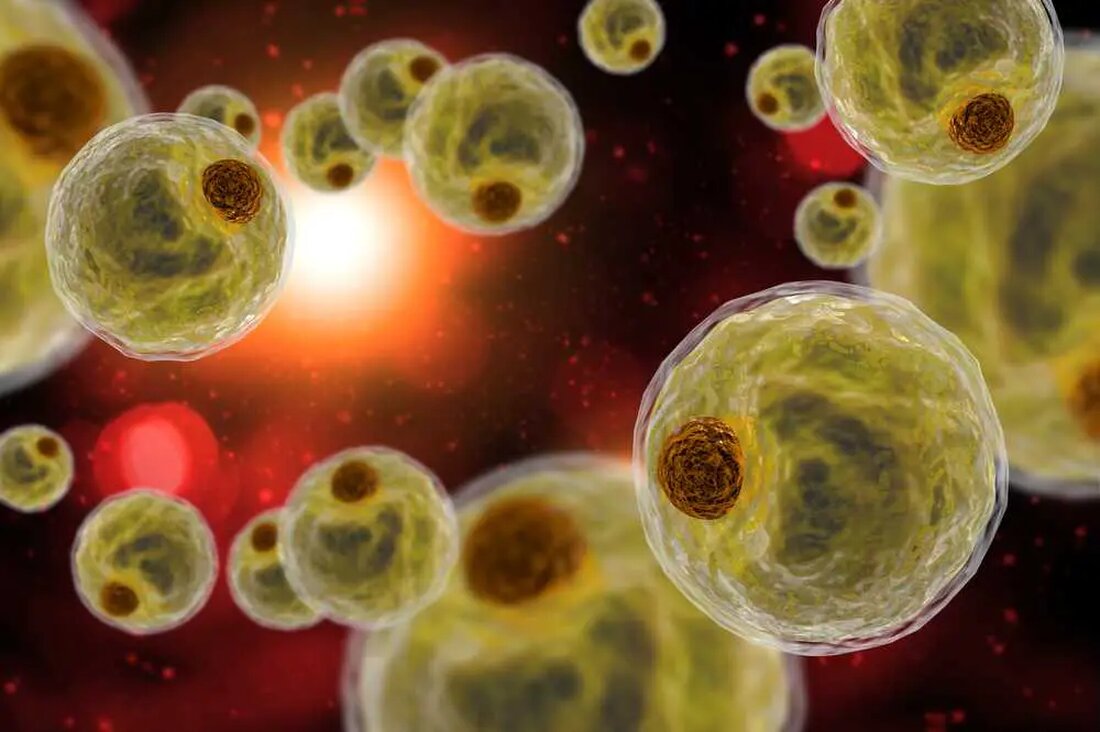
Researchers have recently discovered a new type of smart stem cell known as induced multipotent stem cells (iMS). This discovery represents a significant advance in the field of regenerative medicine. iMS cells are derived from human adipose tissue and have demonstrated their impressive ability to adapt and transform in animal studies, demonstrating their potential for tissue repair.
Professor John Pimanda from UNSW Medicine & Health explains that iMS cells are unique in their ability to respond to their environment. The fact that stem cells are able to respond to their environment and adapt to repair damaged tissue is a novel idea and could lead to a paradigm shift in stem cell research and treatment strategies.
Creating smart stem cells is done by exposing human fat cells to a mixture of compounds. This causes the cells to lose their original identity and behave like stem cells. Interestingly, these reprogrammed cells remain inactive until injury occurs. The cells then adapt and transform into the tissue needed for repair.
The iMS cells have numerous advantages in regenerative medicine. They respond to their environment like chameleons by reacting to local signals and blending seamlessly into the tissue being healed. In contrast to other stem cell technologies, iMS cells are not limited in their regenerative abilities and do not pose any risks such as the development of tumors. Because they are derived from the patient's own tissue, they significantly reduce the risk of rejection. iMS cells have also shown the ability to adapt to different tissue types in mice, making them a type of “smart stem cell.”
The process of converting fat cells into iMS cells is fascinating. By using a blood cancer treatment drug called azacitidine and a natural growth factor that stimulates cell growth and tissue repair, the cells lose their identity as fat cells after about three and a half weeks. This process can be carried out either outside the body in an incubator or inside the body using a mini pump. The latter enables the targeted generation of new, intelligent stem cells near the body part to be repaired.
Although this discovery is exciting, translating the results to human therapy requires extensive research and clinical trials to ensure its safety and effectiveness. Translation from laboratory to clinical use can take many years. Still, iMS cells are promising and could usher in a new era of healing. They offer the possibility of treating degenerative diseases such as Parkinson's and Alzheimer's, injuries caused by accidents or sporting activities and even age-related problems. Additionally, they could minimize ethical concerns often associated with the use of embryonic stem cells.
The future of regenerative medicine seems promising with iMS cells. Their potential to respond to their environment and repair various types of damaged tissue is a breakthrough in this field. Although the road to fully realizing their potential will be long and challenging, the prospects are too significant to ignore. With further research, these “smart” stem cells could be widely used in clinical applications in the future.

 Suche
Suche
 Mein Konto
Mein Konto
