Ultra-precise 3D maps of cancer cells reveal the secrets of tumor growth
Ultra-precise 3D maps of cancer cells decipher how tumors grow and offer new approaches to therapies.
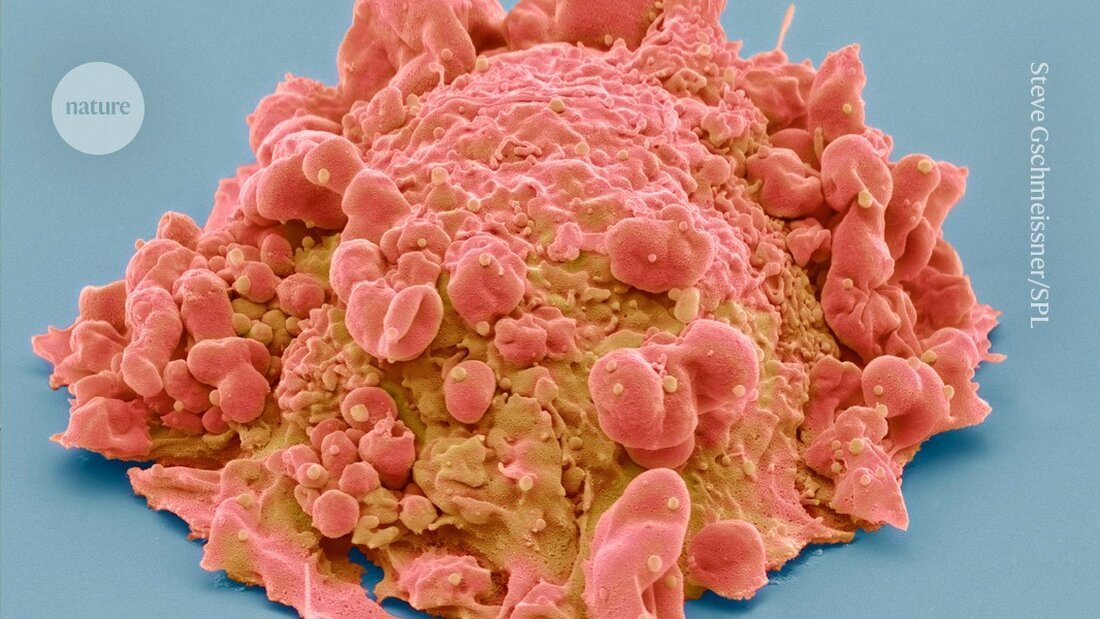
Ultra-precise 3D maps of cancer cells reveal the secrets of tumor growth
Detailed maps that precisely depict the locations of cells in tumors and examine the tumors' biology offer new insights into the development of several types of cancer - including breast, colon and pancreatic cancer - and could provide clues to potential treatments.
In a series of 12 studies, published October 30 in the journal Nature, researchers from the Human Tumor Atlas Network (HTAN) analyzed hundreds of thousands of cells from human and animal tissue. Some of the studies describe 3D maps of cells – known as cell atlases – in tumors, while others create “molecular clocks” that track the cellular changes that lead to cancer.
“Applying these novel tools to cancer allows us to look at it from a different perspective,” says Ken Lau, a computational cell biologist at Vanderbilt University Medical Center in Nashville, Tennessee, and co-author of a study documenting the time course of cellular events in the development of colorectal cancer 1. “We can actually see things we couldn’t see before.”
Mapping tumors
In some of the studies, researchers created atlases that allowed them to study tumors at the single-cell level and investigate how cancer develops. A team analyzed the organization of cells in 131 samples from six different types of cancer, including breast, colon, pancreatic and kidney tumors 2. The scientists found that different regions of the same tumor could respond differently to drugs. Understanding how different cell groups respond to treatments could help develop more effective therapies.
Other studies used 3D mapping to examine samples of colon polyps - abnormal growths in the intestinal lining that can become cancerous. They identified molecular changes in the cells of the polyps, including loss of DNA connections and changes in gene activity 3, as well as changes in immune response, cell growth and hormone metabolism 4, which can occur early and cause the polyp cells to become malignant.
Therapies that target these changes could make cancer treatments and early health interventions more effective, says Ömer Yilmaz, a stem cell biologist at the Massachusetts Institute of Technology in Cambridge. "The best treatment for cancer is prevention. And if we can understand how different cell populations respond to the environment and diet, how this affects tumorigenesis, and how different clones contribute to this process, this could lead to better prevention or detection methods."
Insights into immunity
Other atlases provide clues as to why some cancers are more difficult to treat than others. "Tumors aren't just made up of cancer cells," says Daniel Abravanel, a physician-scientist at the Dana-Farber Cancer Institute in Boston, Massachusetts, and co-author of a study on breast cancer 5. For example, immunotherapies that do not directly target cancer cells, but support the immune system to eliminate them, less effective against breast cancer than other types of cancer, he adds.
To find out why, Abravanel and his colleagues created a 3D tumor atlas using dozens of samples from 60 people with aggressive forms of breast cancer. They looked at how immune cells were distributed and found that some types of immune cells were more common in certain tumors, particularly in people who had received immunotherapy.
In three people, biopsies taken from the same tumor 70-220 days apart showed differences in the amounts of immune cells known as T cells and macrophages. In two cases the number of these cells had decreased over time, while in the third case it had increased.
"This really shows how dynamic the immunological microenvironment is and may explain why attempts to characterize tumors and predict responses to immune checkpoint therapies from a biopsy at a single time point have yielded inconsistent results," says Brian Lehmann, a breast cancer researcher who specializes in genomics at the Vanderbilt-Ingram Cancer Center in Nashville, Tennessee.
In another study, researchers found that some aggressive subtypes of breast cancer contained more immune cells than others and appeared to become "muted" over time 6. These cells expressed a protein called CTLA4, which limits their ability to respond to tumors. Therapies targeting CTLA4 have shown promising results in the treatment of melanoma and lung cancer. “This opens up additional possibilities for the use of this therapy in a subset of breast cancers,” says Lehmann.
CRISPR watch
Other experiments show how cells become cancer cells in the first place. In the colorectal cancer study, Lau and his colleagues developed a "molecular clock" to track how normal cells begin to proliferate uncontrollably in the intestine 1. They used single-cell analysis and a gene editing tool (CRISPR) to create mutations in each cell's DNA. These mutations acted as time stamps, documenting the course of changes and divisions of each cell.
Lau and his team applied this approach to 418 human colon polyps and found that up to 30% of the polyps came from multiple cell types rather than a single cell. In 60% of polyps, one group of cells began to “overtake” others as the polyp grew – leading to the formation of a tumor. Two similar studies in mice 7, 8, including an analysis of 260,922 single cells from 112 samples of intestinal tissue, also showed that a mixture of cells collectively initiate colorectal tumors.
These results challenge previous thinking that colon cancer arises from single, unregulated cells in the intestinal lining and may open up new opportunities for early diagnosis and intervention.
"To assess the risk of [precancerous growths], people use size. The larger the tumor, the higher the risk," says Lau. But the molecular clock and other analyzes show that “there may be other biomarkers that involve genetics and evolution.”
-
Islam, M. et al. Nature https://doi.org/10.1038/s41586-024-07954-4 (2024).
-
Mon, C.-K. et al. Nature https://doi.org/10.1038/s41586-024-08087-4 (2024).
-
Zhu, Y. et al. Nature Cancer https://doi.org/10.1038/s43018-024-00823-z (2024).
-
Esplin, E.D. et al. Nature Cancer https://doi.org/10.1038/s43018-024-00831-z (2024).
-
Klughammer, J. et al. Nature Med. https://doi.org/10.1038/s41591-024-03215-z (2024).
-
Iglesia, M.D. et al. Nature Cancer https://doi.org/10.1038/s43018-024-00773-6 (2024).
-
Sadien, I.D. et al. Nature https://doi.org/10.1038/s41586-024-08053-0 (2024).
-
Lu, Z. et al. Nature https://doi.org/10.1038/s41586-024-08133-1 (2024).

 Suche
Suche
 Mein Konto
Mein Konto
